Opioid Epidemic Statistics
What Are Opioids? How Do Opioids Work?
Opioids are substances that attach to endorphin receptors in the nervous system. Is heroin an opiate or opioid? Opiates are a subcategory of opioids which are made from the opium poppy, these include morphine, codeine, and heroin. Opioids which are not made from opium include methadone and fentanyl, they are fully synthetic.
Throughout the central nervous system, the brain, and digestive tract, embedded in the cell membrane, there are protein receptors with a particular shape called opioid receptors. Endogenous substances called endorphins bind to these receptors and cause a reduction in the release of pain-transmitting and excitatory neurotransmitters like substance P and glutamate. While these neurotransmitters are crucial for the transmission of pain and reducing them reduces pain, they are also crucial for memory and that’s why opioids can cause memory loss. Opioids bind to these proteins, sometimes with far greater intensity than endogenous opioids. This causes a high as excitatory neurotransmitters are inhibited, combined with a tickling of dopaminergic receptors in the nucleus accumbens. Explore additional details at this location: https://www.methadone.org/
Opioids medication list
- Natural
- Codeine
- Opium
- Thebaine
- Morphine derivatives
- acetylpropionylmorphine
- desomorphine
- diacetyldihydromorphine
- diacetylmorphine
- dibenzoylmorphine
- dipropanoylmorphine
- nicomorphine
- Semi-Synthetics
- oxymorphone
- oxycodone aka Oxycontin
- hydromorphone
- hydrocodone
- ethylmorphine
- buprenorphine aka Subutex
- Synthetics
- dextropropoxyphene
- fentanyl
- levorphanol
- methadone
- pethidine
- tapentadol
- tramadol
Opioid addiction and dependence: opioid replacement therapy
How opioid addiction occurs:
In the early 2000s, marketers of the new drug Oxycontin were looking for ways to increase prescriptions of their blockbuster drug. At the same time, professional medical standards organizations and medical professionals added a new vital sign: pain. They would ask patients to rate their pain on a simple scale, often using smiley and sad faces. Studies had shown that pain was being inadequately treated. Some studies showed that pain in minorities was disbelieved and virtually ignored (Trawalter, Hoffman, and Waytz).
Marketers began telling doctors that opioids, which were previously seen to be something to be used only in cancer patients with severe pain and for palliative care for the dying, could be used in chronic pain and minor injuries. Oxycontin was marketed as safe and non-addictive. Prescriptions skyrocketed. Fast forward to 2017, in Alabama, doctors wrote 107.2 prescriptions for opioids for every 100 people. They have more opioid prescriptions than they have people, and at a time when heroin and fentanyl have already replaced prescription opioids as the drug of choice in the United States.

A prescription like Oxycontin comes in your standard prescription pill bottle. It may say take 1 tablet (10 mg) every 12 hours for pain.
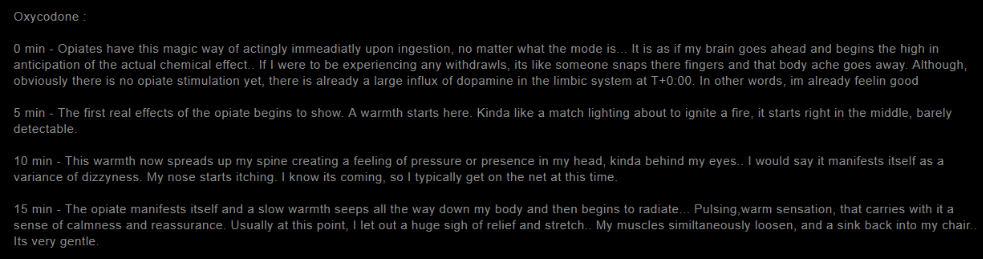
Figure 1.
The Erowid user above described the feeling of warmth and well being upon ingestion of a dose of 40 mg of Percocet at one time. One may have a prescription that lasts a month or less. However, opioid tolerance begins to build. You need to take more opioids to get the same effect, that warmth, pain relief, and feeling of happiness and relaxation. As opioid tolerance sets in, it can take extremely high doses to merely stave off withdrawal.
When doctors recognized that the individual has become addicted due to seeing drug-seeking behavior, begging for dose increases, claiming they lost their prescription bottle and need another, or making up new pains, especially back pain: they may cut the user off completely. At this point, they can experience severe withdrawal symptoms. Many people claim they feel like they are dying. There are flu-like symptoms, dread, anxiety attacks, nausea, vomiting, sweating, and muscle aches. There can be loss of bowel and urinary function causing embarrassing accidents. This can affect the ability to function at work and school. It can ruin relationships. People started buying pills off the street when the doctor cut them off. Some start running scams and black-market businesses involving taking a trip to Florida or another place with lax drug laws and hitting doctor offices known as ‘pill mills’. These businesses may claim to be pain management clinics when what they actually do is prescribe large amounts of opioids at high prices. The users buy it cash only, they may use some, and sell others to make enough profit to make another trip and do the same thing. They typically claim to have back pain or some other type of pain that cannot be objectively discovered. Many of them have actual pain but their drug-seeking behavior is caused mainly by addiction at this point. They get their prescriptions and drive back to Kentucky or Alabama, two of the hardest-hit states, and there disperse, distribute, and use their opioid drugs: Oxycontin, Hydrocodone, hydro codeine, Roxicontin.
After a month of using one of these drugs daily, one will have developed a physical addiction. Whether one develops such an addiction depends on one’s particular physiology and one’s habit of using. With some of these drugs, a physical dependence can develop rapidly, others slower. Heavy and escalating use over a month of time will cause some amount of physical addiction. But the truth is, most people experiment for a long time, years before developing an addiction. They have many chances to turn away, and they do, for a short amount of time, then they may go back to it when life gets stressful.
Now, this has occurred in high numbers of people by 2009. Lots of people are buying pills off the streets, but now pill mills are getting shut down, doctors are cutting people off. People are going to methadone clinics for treatment only to find they are now addicted to a more addictive drug and it’s not cheap at all. Often you have to pay daily in cash. And a new evil is about to be introduced. People have discovered they can buy heroin cheaper and it lasts longer than the pills. Heroin from Mexico now floods the American market. And it is adulterated with fentanyl and carfentanil, a powerful opioid used to tranquilize elephants. Now people are addicted to heroin and fentanyl and overdose deaths are on the rise all around the country. A few people have been able to get out of their addiction using the herb kratom, but authorities have made attempts to ban the herb as it is a threat to methadone treatment centers and pharmaceutical companies who are producing ever more powerful opioids.
Benzodiazepines drugs
Methadone, used in opioid replacement therapy, generally does not cause a strong dopaminergic high, but it does cause a high alone. Yet, when combined with benzodiazepines like Xanax and Klonopin, methadone can produce a high similar to that of heroin. Many people on methadone opioid replacement therapy begin taking benzodiazepines with it to chase the high. Benzodiazepines are also combined with other opioids to increase the high. Benzodiazepine drugs are typically used to treat anxiety. But because of this abuse, doctors begin to reign in benzodiazepine prescriptions. It used to be something easy to get from a primary care provider, now even psychiatrists are wary of prescribing benzodiazepines, except for people of higher status who can pay out of pocket and are deemed more responsible than less successful sufferers. What this is costing society in lack of effective treatment for anxiety disorders is yet to be addressed by medical professionals.
What are the symptoms of opiate withdrawal?
Now when opioid levels run low or one is cut off from opioids, withdrawal set in.
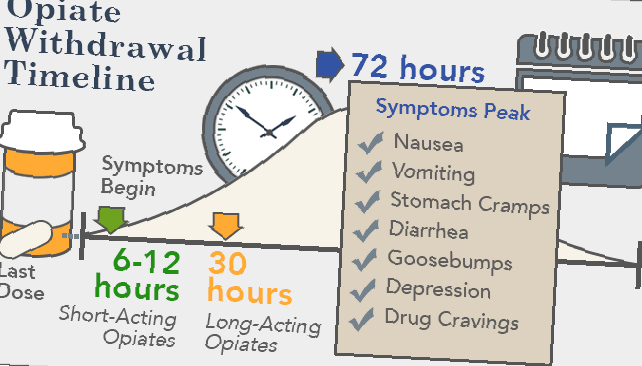
Figure 2.
As you can see, for short-acting opioids, withdrawal can set in just 6 to 12 hours after the last dose. Short-acting opioids are some of the most addictive prescription drugs because withdrawal sets in so quickly and the high hits at one time and can be more intense.
Short-acting opioids (immediate-release forms)
- codeine
- hydrocodone oxymorphone
- hydromorphone
- morphine sulfate
- oxycodone
For long-acting opioids like the fentanyl patch, it can take one or two days for the withdrawal to set in.
Long-acting opioids
- MethadoneLevorphanol
- Opana ER (oxymorphone)
- Duragesic (fentanyl patch)
Physical symptoms of withdrawal include nausea, vomiting, muscle pain, diarrhea, goosebumps, cravings, and teary eyes. However, the psychological effects are damning. There is a sense of dread, paranoia, feeling like you are dying, and physical/psychological (somatic) pain in the back, neck, and other body parts. There is very low energy and inability to perform at work, school, or in relationships. Life stops until you get that next dose. Those in withdrawal are miserable.
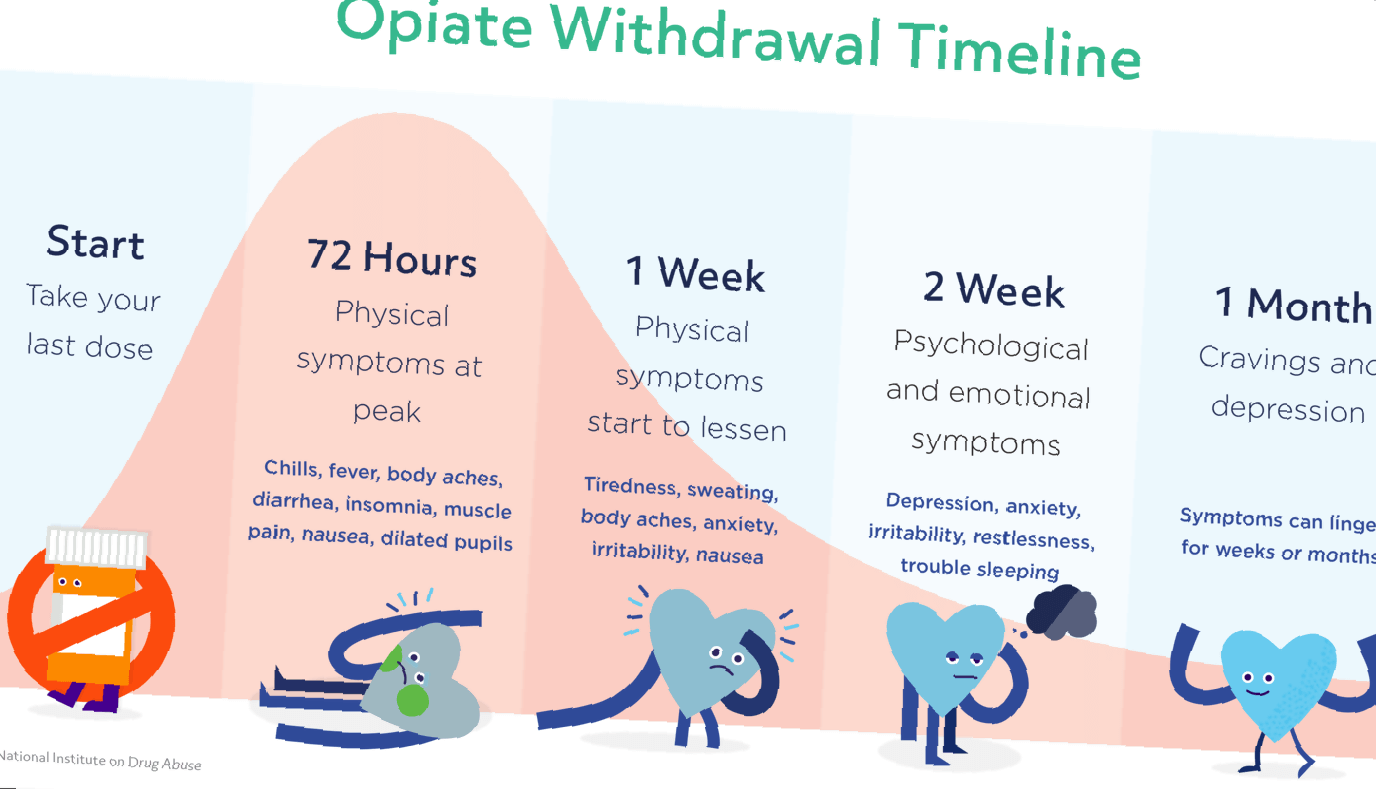
Symptoms peak on day 3, then start to lessen. However, then you have to deal with another obstacle, PAWS.
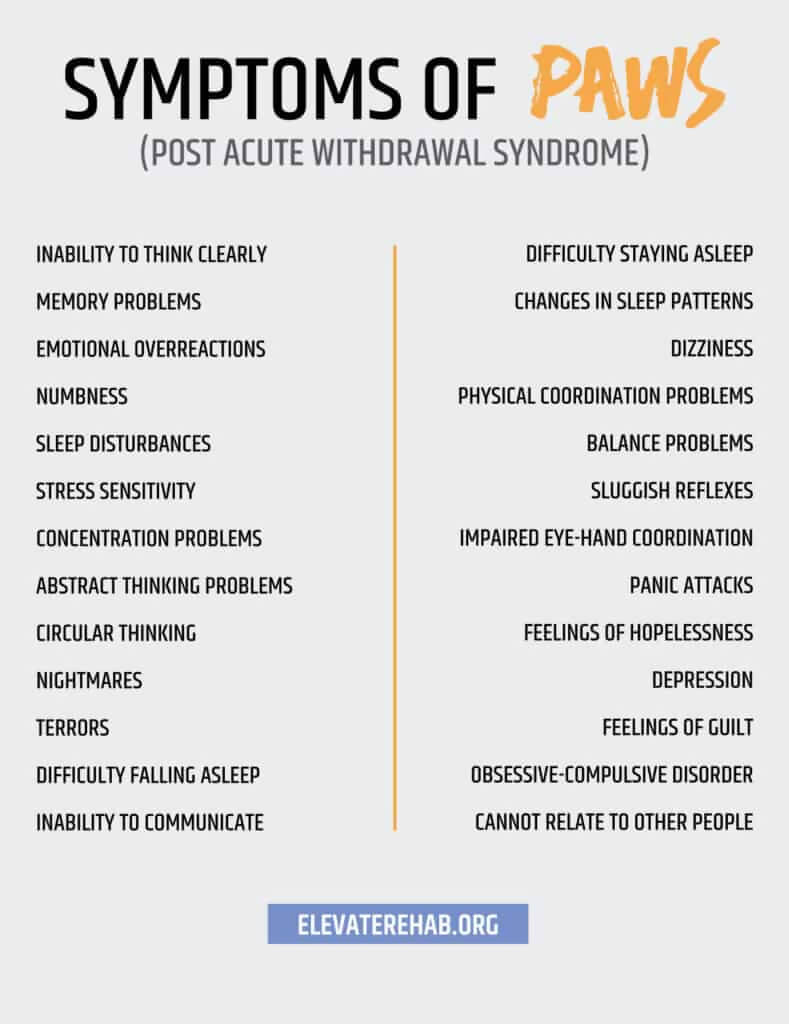
Post-Acute Withdrawal Syndrome (PAWS)
After an opioid has been withdrawn from acutely, the former user can experience symptoms of depression, panic attacks, cravings, and brain fog which can last for up to 2 years. Many people experience PAWS as depression and may seek out treatment. Others just bear with it or take kratom to take the edge off the boredom and suppressed novelty-seeking. If you have PAWS, you should seek professional medical treatment, possibly for a mood disorder. If you seek treatment for former drug addiction, you might be put on an addictive opioid like methadone or buprenorphine, so be careful. If you have gotten off your opioid of choice, you’re in the clear, you don’t want to use opioid replacement therapy to treat PAWS. Opioid replacement therapy is for those who are still addicted, and a good clinic will check to make sure you have opioids in your blood when you come for intake. If you are not using opioids but have PAWS, instead, seek treatment for anxiety or depression.
The basic principles of drug addiction treatment
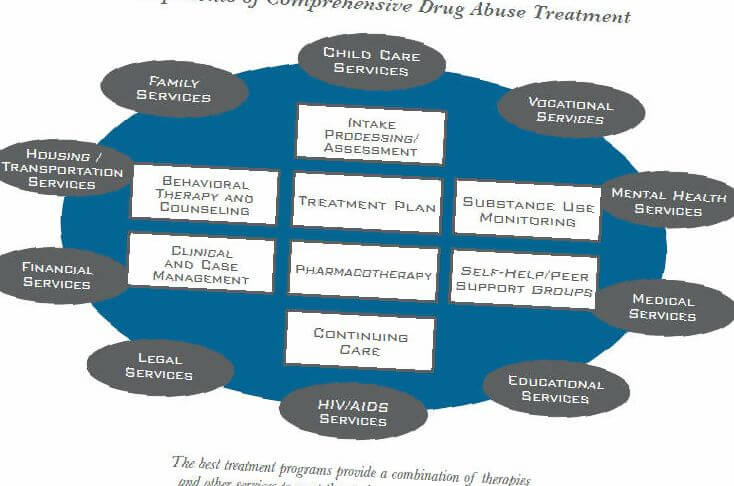
Figure 3.
Behavioral Therapy and Counseling
Cognitive-behavioral therapies and other types of therapy can be used to address several facets of drug addiction. These are talk therapies where a trained and often drug addiction certified therapist talks to the client about things like triggers, when they happen, and how to avoid them. These therapies may address many parts of the patient’s life, such as schooling and relationships. The therapist will help the patient address problematic thoughts and behaviors that lead to and maintain drug addiction. The therapist may also address past traumas which may be reinforcing drug use.
Group Therapy
Group therapies like 12 step programs are a mainstay of addiction treatment. Being in a group of people affected by the same problems provides social reinforcement, companionship, and affection which is often needed to address past traumas suffered by the drug user.
Medication Treatment
We have discussed methadone and buprenorphine treatment. These are referred to as opioid replacement therapies. This can also be done by replacing the drug of choice with a doctor-prescribed brand of the exact same drug, in measured doses, and overseen by a professional. For example, heroin addicts can go to a clinic and get a prescribed dose of heroin which is safer than what they would get on the street. These programs have shown reduced criminality, addiction, overdose, and problem behaviors. Many have proven just as effective as methadone and buprenorphine treatment. This suggests it is the environment around the drug-taking that improves outcomes. You don’t have to get it off the street, the price is controlled, the dose and surroundings are controlled and that alone leads to better outcomes. Without further treatment, most addicts eventually wean off and get clean. With all drugs, most addicts discontinue use without treatment, this is a little known fact that will not be touted by those selling treatment services. Though it may take years, drug use eventually runs its course and the neurons become so biased, they can no longer be abused or some health matter makes quitting mandatory.
Naltrexone
Naltrexone is an opioid antagonist sometimes used in therapy for opioid abuse. It blocks the opioid receptors and makes it impossible to get high from opioids. However, it can sometimes lead to a condition called precipitated withdrawal, where the opioid user is dosed with naltrexone and goes into immediate and intense opioid withdrawal. This can also happen with buprenorphine alone or buprenorphine combined with naltrexone (in studies) or buprenorphine/naloxone (Suboxone).
Naloxone
Naloxone is an opioid antagonist that has prevented countless opioid overdose deaths. It can be sprayed in the nose or injected when a person is suspected to be having an opioid overdose. It will bring them around in minutes. Sometimes, they are angry to have missed their high and now be in withdrawal so there’s a risk without follow up that they will go and overdose again. Naloxone is also combined with buprenorphine (Suboxone) to deter abuse.
Case management
Combinations of behavioral, group, and medication therapies seem to be more effective than either alone. However, those suffering from addiction often have other problems in life that affect their likelihood of relapse. Therefore, case management to help manage financial, occupational, mental health, physical health, and other areas of life affect the chances that the former addict will be successful in continued abstinence. Case managers may be counselors or social workers and can greatly improve outcomes.
Opioid addiction risk factors
Past substance abuse
Those who have abused other substances in the past are more likely to become addicted to opioids. This can include addiction to alcohol or amphetamines.
Mental Health Disorders
Those who have other mental health disorders like anxiety and depression may be more likely to abuse opioids. Abuse of opioids may be a form of self-treatment for mood disorders, personality disorders, chronic pain disorders, or another disease.
Youth
Young people may be more likely to become addicted to opioids. Lack of experience, education, and novelty-seeking may place younger people at higher risk.
Environment
People who grow up in stressful environments or environments that feature drug use may be at greater risk of developing a drug abuse problem. Growing up with parents who suffer from addiction can place one at greater risk. Being in a peer group where one’s peers are users places one at greater risk. During the opioid epidemic in the US, pill use became a social activity among friends. Some users developed an addiction due largely to peer influence.
Dysfunctional family environments can greatly increase the chances of developing a drug addiction issue.
Signs and symptoms of opioid overdose and abuse
When someone is addicted to opioids, you may notice the following symptoms of opioid addiction and opioid side effects:
- Lack of responsibility
- Panic attacks
- Constipation
- Depressed mood
- Drowsiness and nodding
- Euphoria
- Irritableness
- Lack of motivation
- Moodiness
- Vomiting, nausea
- Agitation
- Lack of coordination
- Bad decision making
- Shallow breathing
- Sleeping all the time
- Slurring words
Signs of opioid overdose are a medical emergency (requires administration of naloxone by paramedics or anyone available) and can include:
- Unable to speak
- The body goes limp
- Breathing is weak or has stopped
- Sounds like they are choking or rattling
- Pale face, light sweating
- Lips and fingertips can turn purple or black
- Purplish or grayish skin
- Unconsciousness
- Low, slow, jumpy, or undetectable pulse
- Not responding
- Vomiting and severe nausea
Preventing opioid use disorder and relapse
Clinicians and regulatory authorities have taken many steps to prevent the development of opioid use disorder in the population. Doctors may ask questions about a patient’s use of medication or use screening tools to discover if there may be a problem. They will take note of drug-seeking behavior and requests for escalating doses of opioid medications. Doctors have also decreased their prescribing of new opioid prescriptions, especially for relatively minor ailments. They may look to prescribing less addictive pain relievers like ibuprofen and paracetamol.
State authorities have started tracking prescriptions for various medications in order to prevent doctor shopping, which is when a patient goes to multiple doctors in order to get duplicate narcotic prescriptions for real or fabricated health conditions. This is one means by which those who frequented pill mills were able to get multiple prescriptions that could sell for thousands of dollars on the streets. This was done to make a profit or to support a drug habit.
Patients prescribed opioids or other addictive drugs can guard against addiction by being certain they take their pills and other drugs only as prescribed. It is never okay to use another person’s prescription, even if you think they have the same prescription that you have. If you have concerns that a doctor has prescribed too much medication or for too long a duration, have an honest discussion with your doctor or get a second opinion from another doctor about the risk of becoming physically dependent on your narcotic medication.
Those who are in an environment that could put them at risk for addiction can participate in diversion activities such as sports and exercise. Getting youth involved in church or other group activities can also help keep them focused on positive activities and reduce the chances that they will become involved with drug use. Parents should maintain an open dialogue with their children about drug use and the things that are happening in their peer group.
Once one has gone through drug addiction and gotten some clean time, it’s imperative to guard against relapsing back into drug use. Those with substance abuse disorders have up to a 60 percent chance of relapse. In order to prevent or reduce relapse rates, patients have to be taught to identify and avoid triggers of relapse. Triggers can be something as simple as being in a neighborhood where one recalls engaging in drug use or seeing a certain friend one used to do drugs with. The mind and body may react to these triggers with a feeling of craving and agitation.
Feelings of anxiety or depression may also lead to relapse. Substance abuse disorders are often an attempt to self-treat anxiety or depression. A recurrence of mood disorders in the absence of any way of mollifying that mood can lead to a return to drug abuse. It is, therefore, necessary for those formerly suffering from addiction who are experiencing low or anxious mood to seek treatment from a professional. This can include talk therapy with a therapist and/or pharmacological therapy for mood disorders.
Those with chronic pain may need collaboration between different specialists to fully address pain, anxiety, depression, addiction, and relapse so that none of their conditions are under-treated. Although they may have abused their prescriptions in the past, this does not negate their need for treatment for pain and mood disorders. We want these patients to have faith in their doctors and the medical system. If they do not, they have less incentive to stick to any doctor recommendations. They may reason, I still have pain, why am I paying so much money every visit to get a prescription form of OTC antihistamines for anxiety and pain? They start to feel like the doctor is putting his own needs ahead of theirs in a way that makes it pointless to seek treatment. They may then explore unproven therapies for better or worse.
Many former opioid-addicted persons and people with chronic pain have found relief with herbs like kratom for opioid detox, CBD and medical marijuana for pain, and kava for anxiety. These herbs have been in use for hundreds of years and are widely sold if viewed suspiciously by the pharmaceutical and medical community. It may be worth researching these approaches. Be brave and heal.
Bibliography
Trawalter, Sophie, Kelly M. Hoffman, and Adam Waytz. “Racial bias in perceptions of others’ pain.” PLOS ONE 7.11 (2012). 27 6 2019. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0048546.
- 1 What Are Opioids? How Do Opioids Work?
- 2 Opioids medication list
- 3 Opioid addiction and dependence: opioid replacement therapy
- 4 What are the symptoms of opiate withdrawal?
- 5 Post-Acute Withdrawal Syndrome (PAWS)
- 6 The basic principles of drug addiction treatment
- 7 Opioid addiction risk factors
- 8 Signs and symptoms of opioid overdose and abuse
- 9 Preventing opioid use disorder and relapse